Published 31 August 2023
From Wound to Wellness: Essential Bed Sore Care Tips for Recovery
Understanding Bed Sores
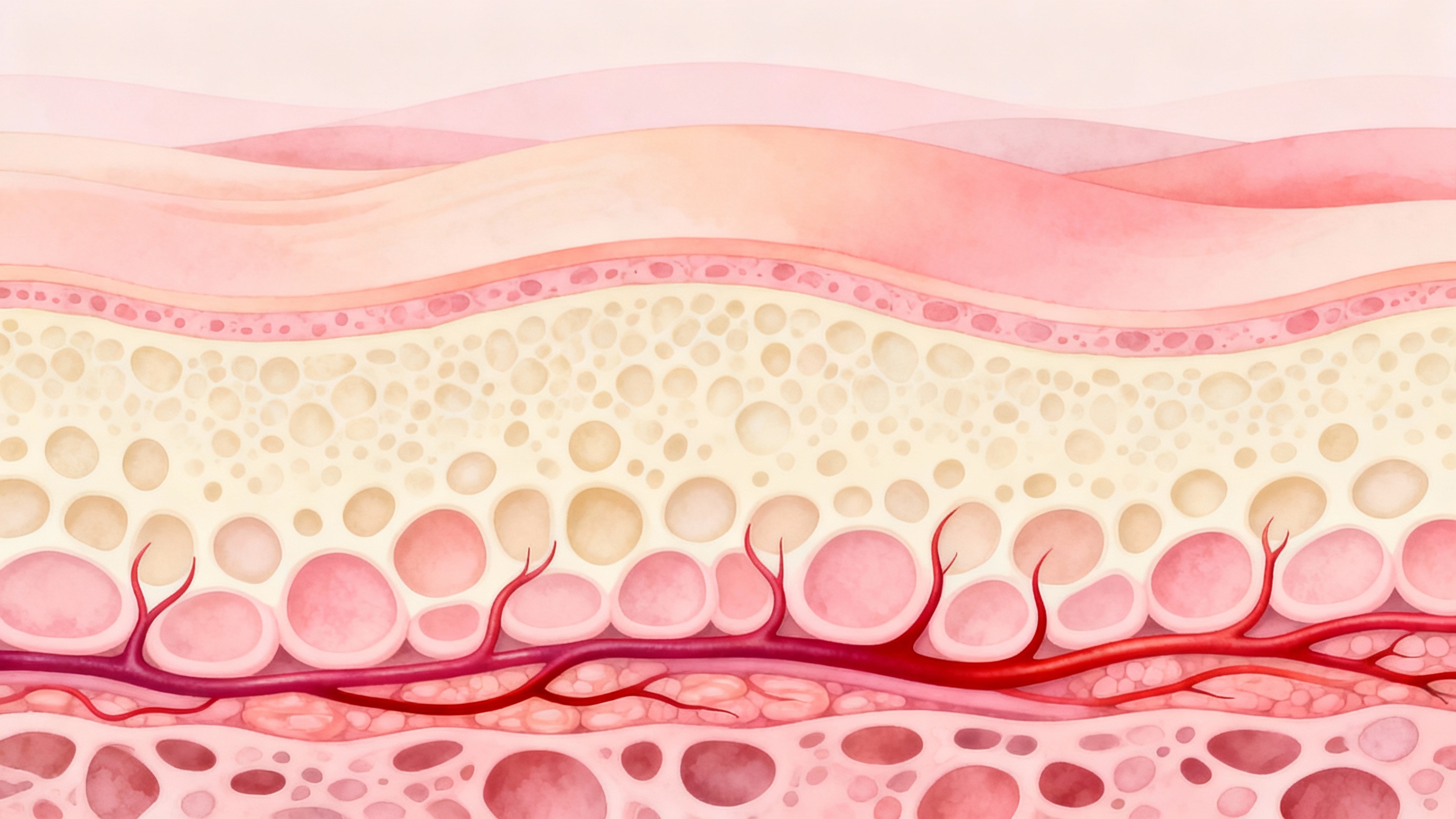
Bed sores, also known as pressure ulcers or decubitus ulcers, are a common concern for individuals who spend extended periods of time in bed or confined to a chair. These sores develop when prolonged pressure on the skin restricts blood flow to a specific area, leading to tissue damage. Understanding the causes, risk factors, and stages of bed sores is essential for effective management and prevention.
What are Bed Sores?
Bed sores are localized injuries to the skin and underlying tissues that occur due to prolonged pressure on specific areas of the body. The pressure inhibits blood flow, depriving the tissues of oxygen and essential nutrients, which can result in tissue damage and the formation of open wounds. Bed sores often occur on bony prominences such as the back, hips, heels, and elbows.
Causes and Risk Factors
Several factors contribute to the development of bed sores. Prolonged pressure is the primary cause, but other factors can increase the risk. These include:
- Immobility or limited mobility, preventing regular changes in position.
- Friction or shearing forces that occur when the skin rubs against surfaces or when there is sliding or dragging of the body.
- Moisture from excessive sweating or incontinence, which can soften the skin and make it more susceptible to damage.
- Poor nutrition and hydration, as inadequate intake of nutrients can impair the body’s ability to repair damaged tissues.
- Medical conditions such as diabetes, vascular disease, and impaired circulation, which can compromise the skin’s ability to receive adequate blood flow.
Stages of Bed Sores
Bed sores are categorized into different stages based on the severity of tissue damage. The stages are as follows:
| Stage | Description |
|---|---|
| Stage 1 | The skin appears red and may feel warm to the touch. The affected area may be slightly swollen or tender but does not have an open wound. |
| Stage 2 | The skin breaks open or forms a blister, shallow crater, or abrasion. The wound is superficial but extends into the deeper layers of the skin. |
| Stage 3 | The wound extends into the subcutaneous tissue, creating a deep crater. Fat may be visible, but muscle, bone, or tendons are not exposed. |
| Stage 4 | The wound is deep, reaching the muscle, bone, or tendons. The surrounding tissue may be necrotic (dead) and require surgical intervention. |
| Unstageable | The wound is covered by eschar (a thick, dry, black or brown scab) or slough (a soft, moist, yellow or white tissue), making it difficult to determine the stage. |
Understanding the stages of bed sores is important for proper assessment, treatment, and monitoring of the healing process. If you’re interested in learning more about preventing bed sores, our article on preventing pressure sores provides valuable information.
By understanding what bed sores are, their causes and risk factors, as well as the stages of their progression, individuals can take proactive steps to manage and prevent these painful and potentially serious wounds.
Essential Bed Sore Care Tips
When it comes to caring for bed sores, there are several essential tips that can help facilitate the healing process and provide relief. These tips focus on proper wound cleaning and dressing, promoting healing with pressure redistribution, and managing pain and discomfort.
Proper Wound Cleaning and Dressing
Keeping the bed sore clean is crucial for preventing infection and promoting healing. To clean the wound, it’s important to use a gentle cleansing solution recommended by a healthcare professional. Avoid harsh soaps or antiseptics that can irritate the skin. Gently cleanse the area with a soft cloth or sterile gauze, being careful not to apply excessive pressure.
After cleaning, it’s essential to apply an appropriate dressing to protect the wound and promote healing. The choice of dressing will depend on the stage and severity of the bed sore. It’s recommended to consult a healthcare provider for guidance on selecting the most suitable dressing. For more information on bed sore dressings, refer to our article on bed sore dressings and bandages.
Promoting Healing with Pressure Redistribution
Pressure redistribution is key to promoting healing and preventing further damage to the affected area. By relieving pressure on the bed sore, blood flow is improved, allowing nutrients and oxygen to reach the wound, aiding in the healing process. Various techniques can be employed to redistribute pressure, such as:
- Frequent repositioning: Regularly changing positions helps to alleviate pressure on specific areas. This can be done by shifting body weight or using specialized equipment like pressure-relief cushions or mattresses.
- Proper bedding and support surfaces: Using supportive cushions, mattresses, or overlays can help distribute pressure more evenly, reducing the risk of additional pressure sores. For more information, check out our article on bed sore cushioning options.
- Managing pressure ulcers at home: Creating a supportive environment at home, including appropriate seating and bedding options, can assist in managing pressure ulcers. Learn more in our article on managing pressure ulcers at home.
Managing Pain and Discomfort
Bed sores can cause significant pain and discomfort. Managing these symptoms is crucial for the well-being of individuals with bed sores. Here are some strategies that can help:
- Relieving pressure on affected areas: As mentioned earlier, redistributing pressure through repositioning and using pressure-relief equipment helps alleviate pain. Additionally, using cushions or pillows to support the body’s natural alignment can provide relief. Find more tips in our article on relieving pressure on affected areas.
- Reducing inflammation: Applying cold compresses or using anti-inflammatory creams can help reduce inflammation around the bed sore. Consult with a healthcare provider to determine the most appropriate method to reduce inflammation. For more information, refer to our article on reducing inflammation in pressure ulcers.
- Using soothing creams: Applying soothing creams or ointments recommended by a healthcare professional can help relieve itching and provide moisture to the affected area. Learn more in our article on soothing creams for pressure ulcers.
By following these essential bed sore care tips, individuals can promote healing, reduce discomfort, and ensure proper wound management. However, it is important to seek professional help for an accurate diagnosis and appropriate treatment options. For more information on seeking professional help and available therapies, refer to our article on bed sore treatment options.
Maintaining Skin Health
When it comes to managing and preventing bed sores, maintaining the health of the skin is of utmost importance. Proper care and attention can help minimize the risk of developing bed sores and promote the healing of existing wounds. In this section, we will explore three essential aspects of skin health: regular skin inspections, moisture control and hydration, and nutrition for skin healing.
Regular Skin Inspections
Regularly inspecting the skin for any signs of redness, discoloration, or breakdown is an essential part of bed sore care. By conducting frequent skin inspections, you can identify potential problem areas early on and take appropriate measures to prevent the development of bed sores.
During skin inspections, pay close attention to bony prominences such as the heels, elbows, hips, and tailbone. These areas are more prone to pressure and friction, making them susceptible to bed sores. If you notice any changes in the skin, such as redness that does not fade after pressure is relieved, consult a healthcare provider for further evaluation and guidance. For more information on preventing bed sores, visit our article on preventing pressure sores.
Moisture Control and Hydration
Proper moisture control is crucial to maintaining skin health and preventing bed sores. Excessive moisture can weaken the skin’s integrity, making it more susceptible to breakdown. On the other hand, dry skin can be more prone to irritation and cracking.
Keep the skin clean and dry by gently patting it with a soft towel after bathing or if it becomes moist due to sweating or incontinence. Avoid rubbing or applying excessive friction to the skin, as this can cause irritation and damage. It’s also important to ensure adequate hydration by drinking plenty of fluids. Well-hydrated skin is more resilient and less prone to dryness and cracking.
Nutrition for Skin Healing
Proper nutrition plays a vital role in promoting skin healing and preventing the development of bed sores. A well-balanced diet rich in essential nutrients can support the body’s natural healing processes and enhance the health of the skin.
Include foods that are high in protein, vitamins (particularly vitamins A and C), and minerals such as zinc and copper in your diet. Protein is essential for tissue repair and regeneration, while vitamins and minerals help support the overall health and integrity of the skin. Consult a healthcare provider or a registered dietitian for personalized dietary recommendations based on your specific needs.
By prioritizing regular skin inspections, maintaining proper moisture control and hydration, and ensuring adequate nutrition, you can take proactive steps in maintaining the health of your skin and preventing the development of bed sores. Remember, if you have any concerns or questions regarding your skin health or wound care, it’s essential to consult a healthcare provider for proper assessment and guidance. For more information on managing symptoms and relief for bed sores, visit our article on coping with bed sores.
Prevention Measures
Taking proactive steps to prevent bed sores is crucial for maintaining skin health and minimizing the risk of developing these painful wounds. Implementing preventive measures can help individuals with limited mobility or those confined to bed avoid the occurrence of bed sores. Here are three essential prevention measures to consider:
Frequent Repositioning and Pressure Relief
Frequent repositioning is key to preventing bed sores. By regularly changing positions, individuals can alleviate pressure on specific areas of the body, reducing the risk of prolonged pressure on vulnerable skin. It is recommended to reposition at least every two hours, alternating between lying on the back, left side, right side, and sitting up if possible. This practice helps to distribute pressure evenly and promotes blood circulation, reducing the likelihood of bed sores. For more information on preventing pressure sores, check out our article on preventing pressure sores.
Proper Bedding and Support Surfaces
Choosing the right bedding and support surfaces is essential for preventing bed sores. Opt for a mattress or mattress overlay that is specifically designed to redistribute pressure. These specialized surfaces help distribute body weight more evenly, reducing pressure on specific areas. Additionally, the bedding should be clean, dry, and free from wrinkles, as these factors can contribute to the development of bed sores. It is advisable to consult with a healthcare professional or therapist to determine the most suitable bedding and support surfaces for individual needs.
Skin Care Routine for Prevention
Establishing a regular skin care routine is vital for preventing bed sores. The routine should include keeping the skin clean and dry, as well as moisturized. Regularly clean the skin with mild, non-irritating cleansers, and gently pat dry with a soft towel. Moisturizing the skin with a suitable moisturizer helps maintain skin integrity and prevent dryness. It is important to avoid excessive moisture, as prolonged exposure to moisture can increase the risk of skin breakdown. For more information on maintaining skin health, refer to our article on skin health for pressure ulcers.
Implementing these prevention measures can significantly reduce the risk of bed sores. However, it’s important to remember that individual circumstances may vary, and consulting with a healthcare provider is essential for personalized advice and guidance. By being proactive in preventing bed sores, individuals can maintain their skin health and overall well-being.
Seeking Professional Help
While there are various bed sore care tips that can be implemented at home, it is important to know when it’s necessary to consult a healthcare provider. Seeking professional help is crucial to ensure proper assessment, treatment, and management of bed sores. Here are some key considerations:
When to Consult a Healthcare Provider
It is advisable to consult a healthcare provider if you or your loved one develop bed sores or if existing bed sores worsen despite home care efforts. Prompt medical attention is essential for proper evaluation and to prevent the progression of the condition. It is particularly important to seek professional help if any of the following are observed:
- The bed sore is deep, large, or appears infected.
- There is an increase in pain, redness, swelling, or drainage from the wound.
- The surrounding skin shows signs of cellulitis (inflammation) or other signs of infection.
- The individual experiences persistent fever, elevated heart rate, or other systemic symptoms.
Treatment Options and Therapies
Healthcare providers have the expertise to determine the appropriate treatment options and therapies based on the severity and stage of the bed sore. Treatment may involve a combination of medical interventions and wound care techniques, such as:
-
Wound cleaning and dressing: Healthcare providers can provide guidance on proper wound cleaning techniques and recommend appropriate dressings to promote healing. For more information on wound care, refer to our article on bed sore dressings and bandages.
-
Pressure redistribution: Healthcare providers may suggest pressure redistribution techniques and devices to relieve pressure on the affected areas. These techniques aim to promote blood circulation and prevent further damage to the skin. Learn more about relieving pressure on affected areas in our article on relieving pressure on affected areas.
-
Medications: In some cases, healthcare providers may prescribe medications to manage pain, reduce inflammation, or treat underlying infections. It is important to strictly follow the prescribed medication regimen and consult the healthcare provider for any concerns or side effects.
Supportive Resources and Services
Healthcare providers can also provide information and refer individuals to supportive resources and services that can aid in the management of bed sores. These may include:
-
Home healthcare services: Healthcare providers can coordinate with home healthcare agencies to provide specialized wound care and nursing services at home.
-
Physical therapy: Physical therapists can assist in developing personalized exercise and mobility programs to prevent further complications and promote overall well-being.
-
Nutritional support: Healthcare providers may involve dietitians or nutritionists to ensure adequate nutrition for optimal wound healing. Consult our article on nutrition for skin healing for more information.
Remember, seeking professional help is an important step in the comprehensive management of bed sores. Healthcare providers have the knowledge and expertise to provide appropriate care, monitor progress, and address any complications that may arise. Collaborating with healthcare professionals can significantly improve the healing process and overall well-being of individuals with bed sores.
