Published 31 August 2023
Revitalizing Skin Health: Essential Tips for Pressure Ulcers Care
Understanding Pressure Ulcers
Pressure ulcers, also known as bed sores or pressure sores, are a common concern for individuals who are bedridden or have limited mobility. In this section, we will explore what pressure ulcers are, the causes and risk factors associated with them, and the stages of pressure ulcers.
What are Pressure Ulcers?
Pressure ulcers are localized injuries that occur when soft tissues are compressed between a bony prominence and an external surface for an extended period of time. They typically develop in areas where there is constant pressure or friction, such as the heels, hips, tailbone, and elbows.
These wounds can vary in severity, ranging from mild reddened areas to open sores that extend into deeper tissues. Pressure ulcers are often painful and can significantly impact an individual’s quality of life.
Causes and Risk Factors
Several factors contribute to the development of pressure ulcers. Prolonged pressure is the primary cause, but other factors can increase the risk. Some common causes and risk factors include:
- Immobility or limited mobility: Being bedridden or confined to a wheelchair reduces the ability to change positions frequently, leading to prolonged pressure on certain body areas.
- Friction and shear: When the skin rubs against surfaces or when different layers of tissue slide against each other, it can damage the skin and increase the risk of pressure ulcers.
- Poor nutrition: Inadequate intake of nutrients, especially protein, vitamins, and minerals, can weaken the skin and make it more susceptible to damage.
- Moisture: Excessive moisture, such as from perspiration or urinary or fecal incontinence, can soften the skin and increase the risk of pressure ulcer development.
- Age: Older adults are more prone to developing pressure ulcers due to factors such as reduced skin elasticity, slower healing process, and underlying health conditions.
- Chronic medical conditions: Conditions like diabetes, vascular disease, and neurological disorders can impair blood flow and sensation, making the skin more vulnerable to damage.
Stages of Pressure Ulcers
Pressure ulcers are classified into different stages based on their severity. The stages help healthcare professionals assess the extent of tissue damage and determine appropriate treatment. The four stages of pressure ulcers are:
- Stage 1: The mildest form of pressure ulcer, characterized by non-blanchable redness on intact skin. The affected area may feel warm, firm, or soft compared to surrounding tissues.
- Stage 2: In this stage, the skin breaks open, forming a shallow, painful ulcer. The wound may appear as a blister or abrasion, with some skin loss. The surrounding tissue may show signs of inflammation.
- Stage 3: The ulcer extends deeper into the skin, affecting the subcutaneous tissue. The wound may appear as a crater-like cavity with visible fat. Infection risk increases at this stage.
- Stage 4: The most severe stage of pressure ulcers, where the wound extends even deeper into the muscle, tendon, or bone. The wound may have a foul odor, and there is a high risk of infection and tissue necrosis.
Understanding the stages of pressure ulcers is crucial for proper assessment, treatment, and prevention strategies. Regular monitoring and early intervention can help prevent the progression of pressure ulcers to more severe stages. For more information on preventing pressure sores, check out our article on preventing pressure sores.
By understanding the nature of pressure ulcers, their causes and risk factors, and the different stages involved, individuals can take proactive measures to prevent and manage these challenging wounds.
Importance of Skin Health in Pressure Ulcer Care
When it comes to pressure ulcer care, maintaining good skin health is of utmost importance. The condition of the skin plays a crucial role in both the prevention and healing of pressure ulcers. Understanding the role of the skin and being aware of common skin issues in pressure ulcer patients is essential in providing effective care.
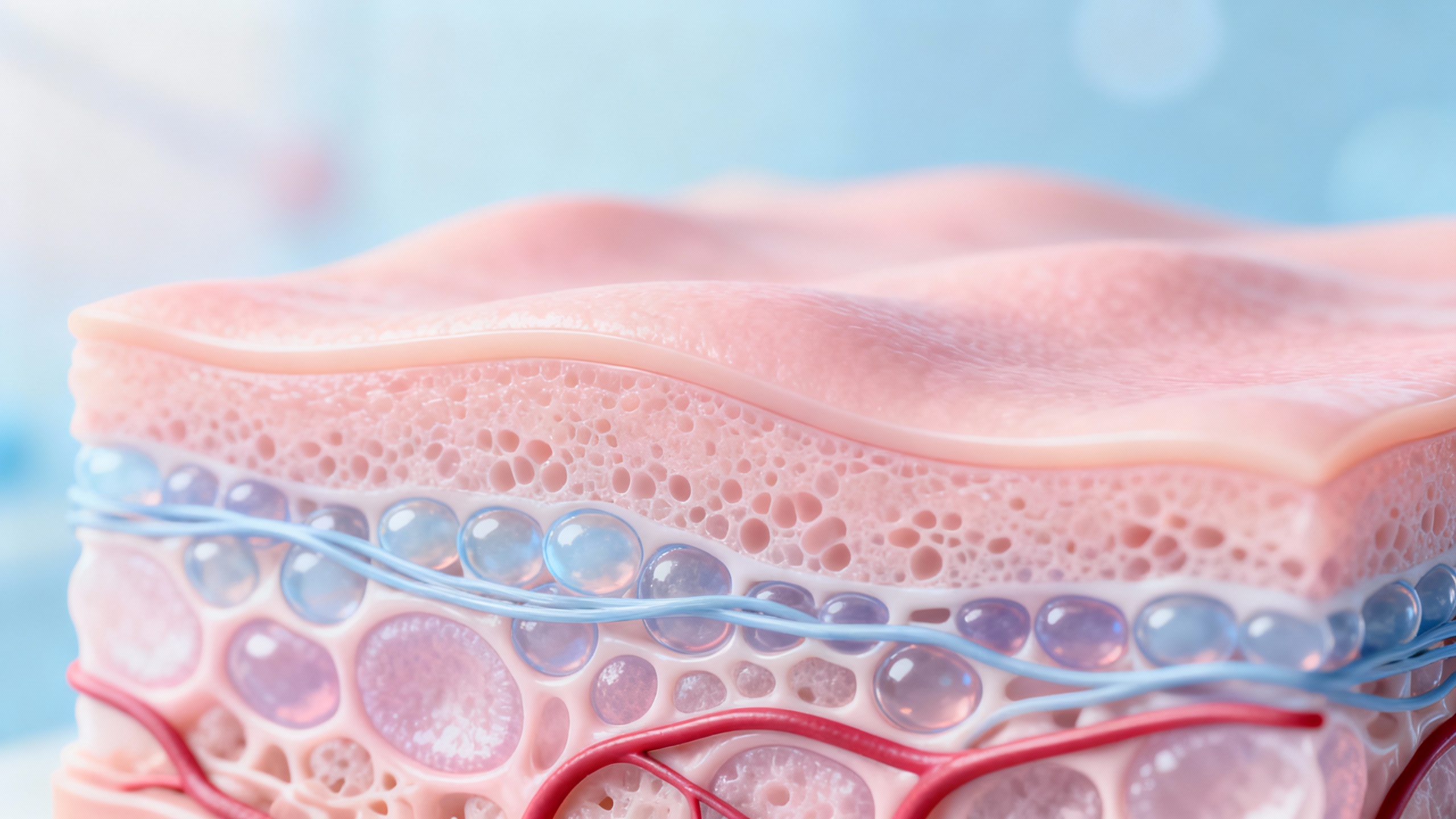
The Role of Skin in Pressure Ulcer Prevention and Healing
The skin acts as a protective barrier against external factors that can lead to the development of pressure ulcers. Healthy skin helps distribute pressure evenly and prevents excessive friction and shearing forces on vulnerable areas of the body. It also plays a vital role in maintaining proper blood flow and supplying nutrients to the underlying tissues.
In pressure ulcer prevention, intact and healthy skin acts as the first line of defense. By keeping the skin clean, moisturized, and free from excessive moisture or dryness, the risk of pressure ulcers can be significantly reduced. Regular inspection of the skin helps identify early signs of pressure ulcers, allowing for prompt intervention. To learn more about preventing pressure ulcers, visit our article on preventing pressure sores.
In the healing process of existing pressure ulcers, healthy skin surrounding the wound plays a crucial role. It provides a conducive environment for new tissue growth and supports the formation of granulation tissue. Proper wound care, including the use of appropriate dressings and bandages, helps protect the surrounding skin and promote healing. For more information on wound care, refer to our article on bed sore dressings and bandages.
Common Skin Issues in Pressure Ulcer Patients
Pressure ulcer patients often experience various skin issues that can complicate the healing process. Some common skin issues include:
1. Skin breakdown and damage: Prolonged pressure, friction, and moisture can lead to skin breakdown, making it more susceptible to pressure ulcers. It is essential to address these issues promptly and take preventive measures to protect the skin.
2. Skin dryness and itching: Dry skin can become itchy and uncomfortable, leading to scratching, which further damages the skin. Proper moisturization is crucial to keep the skin hydrated and reduce itching. For relieving itching caused by bed sores, refer to our article on relieving itching caused by bed sores.
3. Skin infections: Damaged skin is more prone to infections. Bacteria can enter through open wounds or compromised skin, leading to localized infections or cellulitis. Proper hygiene practices and infection prevention measures are vital in minimizing the risk of skin infections.
4. Skin maceration: Excessive moisture from sweating, urine, or wound drainage can cause skin maceration, softening the skin and increasing the risk of breakdown. Regular cleansing and appropriate use of moisture barriers help prevent maceration.
By understanding the importance of skin health and addressing common skin issues, caregivers and patients can work together to provide effective pressure ulcer care. Regular cleansing, moisturizing, and implementing preventive measures are key to maintaining skin integrity. Collaborating with healthcare professionals and seeking their guidance when needed ensures comprehensive care for pressure ulcer patients.
Essential Tips for Maintaining Skin Health
To effectively manage pressure ulcers and promote healing, maintaining skin health is of utmost importance. Here are essential tips to help you maintain the health of your skin:
Regular Cleansing and Moisturizing
Regular cleansing of the skin is essential for preventing infection and maintaining its integrity. Cleanse the affected area gently with mild, non-irritating cleansers and lukewarm water. Avoid scrubbing or using harsh soaps that can strip the skin of its natural oils. After cleansing, pat the skin dry with a soft towel, being careful not to rub or irritate the area.
Moisturizing the skin is equally important to prevent dryness and promote healing. Use fragrance-free moisturizers that are specifically formulated for sensitive skin. Apply the moisturizer gently, using upward strokes, and ensure it is fully absorbed before dressing the wound. Regular moisturizing helps to keep the skin hydrated and supple, reducing the risk of further damage.
Proper Nutrition and Hydration
Maintaining a healthy diet and staying properly hydrated are crucial for skin health. Nutrient-rich foods, including fruits, vegetables, whole grains, and lean proteins, provide the essential vitamins and minerals needed for skin repair and regeneration. Adequate protein intake is particularly important for wound healing. Consult with a healthcare professional or a registered dietitian for personalized dietary recommendations.
Hydration plays a vital role in maintaining the elasticity and moisture balance of the skin. Drink plenty of water throughout the day to keep the skin hydrated from within. Avoid excessive consumption of dehydrating substances such as caffeine and alcohol, as they can contribute to dryness and compromise the skin’s integrity.
Positioning and Pressure Redistribution
Proper positioning and pressure redistribution are essential for relieving pressure on vulnerable areas and preventing the development of new pressure ulcers. If you are bedridden or spend extended periods in a wheelchair, it’s crucial to change positions regularly to alleviate pressure on specific areas. Utilize supportive devices, such as pillows or cushions, to help distribute pressure evenly and reduce the risk of pressure ulcers.
Additionally, consider using specialized pressure-relieving aids, such as foam or gel pads, to provide extra cushioning and support. These aids can help alleviate pressure on bony prominences and reduce the risk of skin breakdown. Consult with a healthcare professional to determine the most suitable pressure redistribution devices for your specific needs.
By following these essential tips for maintaining skin health, you can significantly contribute to the prevention and healing of pressure ulcers. Remember to consult with a healthcare professional for personalized advice and treatment options. For more information on preventing pressure ulcers, visit our article on preventing pressure sores.
Managing Pressure Ulcer Symptoms
When it comes to managing pressure ulcers, there are several strategies that can help alleviate symptoms and promote healing. This section will explore three essential aspects of pressure ulcer management: pain management strategies, wound dressings and bandages, and infection prevention and treatment.
Pain Management Strategies
Pain is a common symptom associated with pressure ulcers. To provide relief and improve comfort, various pain management strategies can be employed. These may include:
- Medication: Over-the-counter pain relievers, such as acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs), can help reduce mild to moderate pain. Prescription medications may be necessary for severe pain management.
- Topical Treatments: Applying soothing creams or ointments, such as those containing lidocaine or hydrocortisone, can help relieve localized pain and reduce inflammation. Visit our article on soothing creams for pressure ulcers for more information.
- Alternative Therapies: Complementary approaches like massage, heat therapy, or transcutaneous electrical nerve stimulation (TENS) may also provide pain relief. Consult with a healthcare professional for guidance on these methods.
It’s crucial to address pain promptly and effectively to ensure the overall well-being and comfort of individuals with pressure ulcers.
Wound Dressings and Bandages
Proper wound management is essential for the healing of pressure ulcers. Wound dressings and bandages play a crucial role in protecting the ulcers from further damage, promoting a moist wound environment, and facilitating the healing process. The choice of dressings and bandages depends on the characteristics and severity of the pressure ulcer.
- Transparent Films: These thin, adhesive dressings are suitable for shallow, non-infected ulcers. They provide a barrier against external contaminants while allowing visualization of the wound.
- Hydrocolloid Dressings: These dressings create a moist environment that supports healing and helps to remove dead tissue. They are commonly used for stage II and III pressure ulcers.
- Foam Dressings: Foam dressings absorb excess moisture and promote a moist wound environment. They are suitable for moderate to heavily exuding ulcers.
- Alginate Dressings: Made from seaweed fibers, alginate dressings are highly absorbent and are ideal for heavily exuding wounds. They facilitate the removal of dead tissue and promote granulation.
- Antimicrobial Dressings: In cases of infected pressure ulcers, antimicrobial dressings may be used to help control bacterial growth and prevent further infection.
The choice of dressing should be made in consultation with a healthcare professional, taking into consideration the individual’s specific needs and the characteristics of the pressure ulcer. For more information on wound care options, refer to our article on bed sore dressings and bandages.
Infection Prevention and Treatment
Infection is a serious complication that can significantly delay the healing process of pressure ulcers. To prevent and manage infections, it is crucial to follow proper hygiene practices and seek prompt medical attention. Some important measures include:
- Cleaning and Disinfection: Regular cleansing of the pressure ulcer with mild soap and water or a sterile saline solution can help prevent infection. Avoid using harsh cleansers or excessive scrubbing, as this can damage the surrounding healthy skin. For more details on wound cleansing, refer to our article on managing symptoms of bed sores.
- Antibiotics: If a pressure ulcer becomes infected, antibiotics may be prescribed to combat the underlying bacterial infection. It is essential to complete the full course of antibiotics as prescribed by a healthcare professional.
- Regular Monitoring: Regular check-ups with a healthcare provider are important to monitor the progress of the pressure ulcer and identify any signs of infection or complications. Early detection and intervention can significantly improve outcomes.
Infection prevention and prompt treatment are critical to ensure the best possible outcome for individuals with pressure ulcers. Collaborating with healthcare professionals and adhering to their guidance is crucial for effective care. For more information on managing pressure ulcers, consult our article on managing pressure ulcers at home.
By implementing these strategies for managing pressure ulcer symptoms, individuals can experience relief and support the healing process. Proper pain management, appropriate wound dressings, and vigilant infection prevention and treatment are essential components of comprehensive pressure ulcer care.
Seeking Professional Help
While there are several measures you can take to maintain skin health and manage pressure ulcers, it is essential to seek professional help for proper care and treatment. Consulting a healthcare provider can ensure that you receive the necessary guidance and support in addressing pressure ulcers effectively.
When to Consult a Healthcare Provider
It is important to reach out to a healthcare provider if you or your loved one develops pressure ulcers or if existing ulcers show signs of worsening. Some indicators that may warrant medical attention include:
-
Increased pain or discomfort: If the pain associated with the pressure ulcers becomes more severe or difficult to manage, it is crucial to seek medical advice. Healthcare professionals can recommend pain management strategies and provide appropriate relief measures. For more information, refer to our article on relieving pain from pressure ulcers.
-
Signs of infection: If you notice any signs of infection, such as increased redness, warmth, swelling, or drainage from the ulcers, it is important to consult a healthcare provider promptly. They can assess the situation, prescribe appropriate antibiotics if necessary, and guide you on infection prevention and treatment. To learn more about treating infected pressure ulcers, refer to our article on treating infected bed sores.
-
Uncontrolled or worsening symptoms: If you have been following recommended care measures but notice that the pressure ulcers are not improving or are getting worse, it is advisable to seek professional help. Healthcare providers can reassess the condition, adjust the treatment plan if needed, and provide additional guidance to promote healing and prevent further complications.
Importance of Regular Check-ups
Regular check-ups with a healthcare provider are crucial for individuals with pressure ulcers. These appointments allow for continuous monitoring of the ulcers’ progress, evaluation of the effectiveness of the treatment plan, and adjustment of care measures as required. It is essential to attend these check-ups as scheduled to ensure proper healing and to address any concerns or questions you may have.
Collaborating with Healthcare Professionals for Effective Care
Collaborating with healthcare professionals is key to effective pressure ulcer care. They possess the expertise and experience to provide guidance tailored to your specific needs. By working together, you can develop a comprehensive care plan that includes appropriate wound dressings, bandages, and other interventions to facilitate healing and reduce the risk of infection. Healthcare providers can also offer advice on managing discomfort, reducing inflammation, and promoting overall skin health.
It is important to actively communicate with your healthcare provider, share any changes or concerns, and follow their recommendations diligently. Remember, a collaborative approach ensures that you receive the best possible care and support in managing pressure ulcers.
In the next section, we will discuss additional tips for maintaining skin health, which can complement the care provided by healthcare professionals. These tips can contribute to the prevention and healing of pressure ulcers in conjunction with professional guidance.
